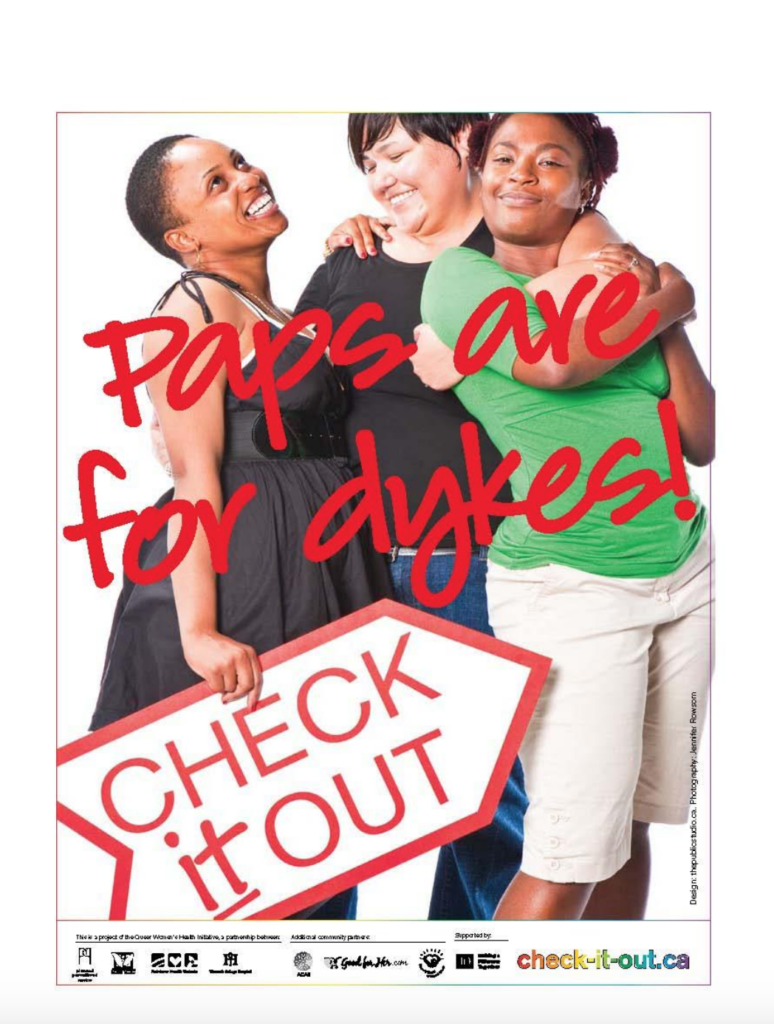
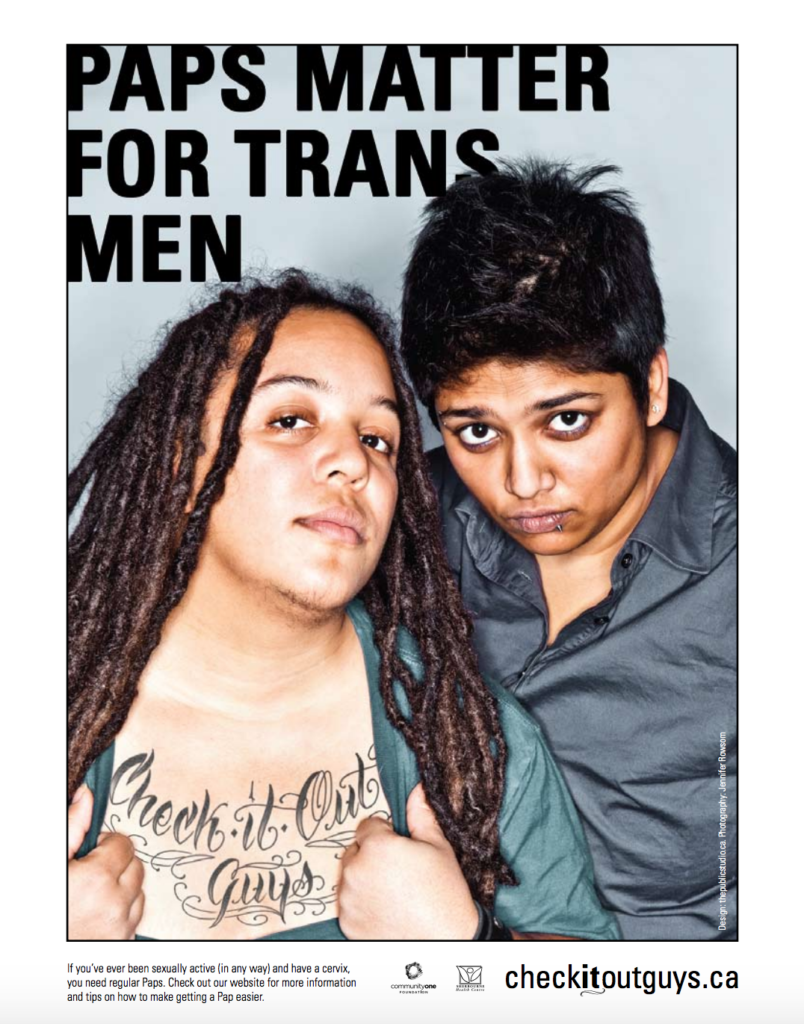
The Check it Out and Check it Out Guys campaigns were launched in 2009 and 2010 respectively by Rainbow Health Ontario and various community partners to raise awareness about the importance of Pap screenings for specific populations. The Check it Out campaign focused on reminding women who have sex with women that Paps matter for them, and Check it Out Guys on the importance of Paps for trans men.
While both websites are no longer active, their full content (last updated in 2009/2010) still remains accessible via the WayBack Machine Internet Archive. Visit the archived Check it Out or Check it Out Guys sites today.
Materials for both campaigns remain available for order in the RHO online store. The URLs on the campaign materials are still active and will bring visitors to this page.